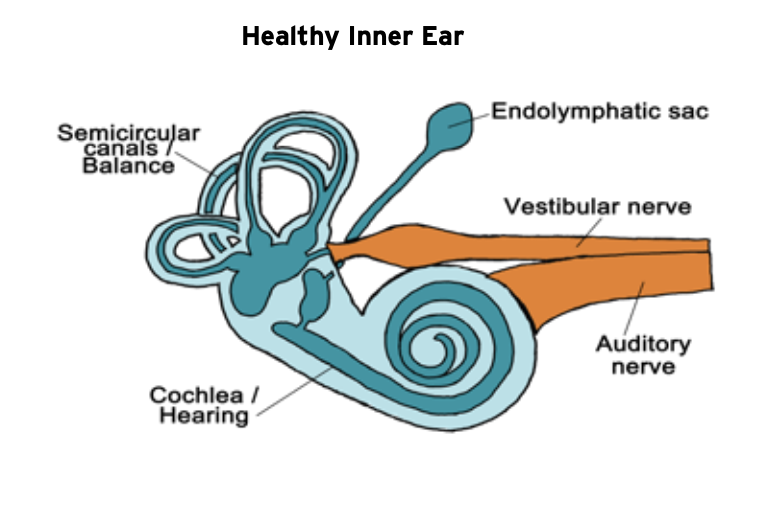
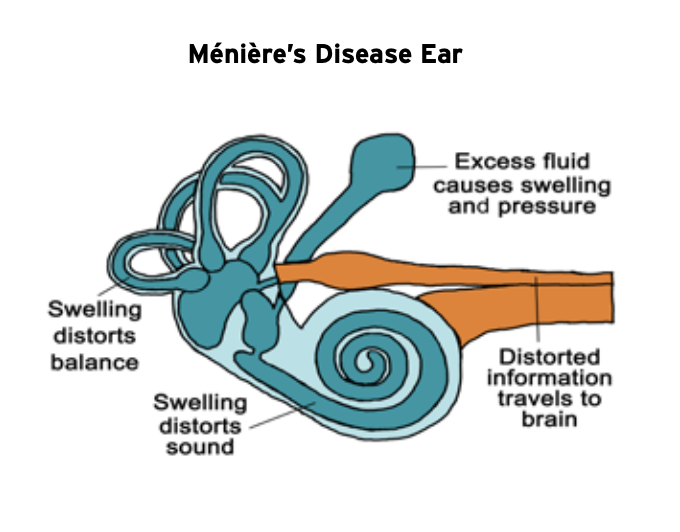
Meniere’s disease is a condition that affects the part of the ear known as the inner ear. The inner ear, which is deep to the ear canal and eardrum, is comprised of two parts. The cochlea is the organ of hearing, and the vestibular labyrinth is a set of tiny organs involved with our sense of balance. Meniere’s disease is part of a larger inner ear disease spectrum known as either hydropic inner ear disease or endolymphatic hydrops. Hydropic inner ear disease is a condition wherein the pressure and volume of the fluid, known as “endolymph”, within the tiny membrane-bound spaces of the inner ear have become elevated and distended, a state known as “hydrops”. Sometimes hydrops is caused by an identifiable injury to the inner ear such as trauma, infection, or an inflammatory disease. However, most cases of hydropic inner ear disease have no clearly identifiable cause. The Meniere’s disease process may cause symptoms such as hearing loss, ear fullness, tinnitus, sound distortion, sound sensitivity, vertigo, imbalance, or sudden falls. Some cases of hydropic ear disease only involve auditory symptoms such as hearing loss and ear pressure; however, when hydropic inner ear disease is associated with multiple bouts of vertigo, it is then referred to as Meniere’s disease.
In the early stages, hydropic inner ear disease is associated with fluctuating ear fullness, hearing loss, and tinnitus (ringing/roaring noise in the ear). These early-stage cases typically have not yet sustained significant permanent damage to the inner ear and the hearing loss is usually only in the low frequency sound range. Initiation of aggressive treatment during this early phase is optimal. If the condition advances, vertigo spells may become more frequent and severe, and the pattern of hearing loss usually spreads to affect all frequencies of sound. Advanced stage Meniere’s disease is associated with more severe and irreversible damage to the hearing and balance organs, to the point where all useful hearing may be lost. Many of the most advanced cases of Meniere’s disease will eventually “burn out”, as vertigo spells cease once the inner ear is damaged enough that most or all balance function is lost in addition to useful hearing.
Meniere’s affects both males and females, with the peak incidence in middle age. It usually causes symptoms in only one ear, but the presence of hydrops in both ears is not uncommon. A typical attack of Meniere’s comes on without warning or any obvious precipitating event. It can range from mild to severe and may last from minutes to hours. The patient will usually notice that hearing in the affected ear becomes muffled and the ear feels “full”. The patient may also experience an increase in noise in their ear and vertigo (a spinning form of dizziness), which if severe can lead to nausea and vomiting. An especially severe Meniere’s variant may include “drop attacks”, where the patient experiences a sudden loss of balance and may fall, although they do not lose consciousness.
The clinical course of hydropic inner ear disease and Meniere’s is difficult to predict and often irregular. Sometimes the condition will flare up and result in severe symptoms and frequent vertigo attacks for several weeks or months. At other times, it will enter a quiescent phase where symptoms are well-controlled and minimal over months to years. There seems to be a sub-group of Meniere’s patients that are impacted by environmental factors such as the weather. In particular, major shifts of barometric pressure into the severely low range have been documented to worsen symptoms. Further, general health issues may impact a hydropic ear such as obstructive sleep apnea, intracranial hypertension, or systemic inflammation within the body. For example, a major flare up of allergies, Covid-19, or anything that would prompt excessive bodily fluid retention could potentially exacerbate symptoms.
Some individuals who appear to have Meniere’s disease may in fact have a migraine variant known as vestibular migraine, which can mimic some of the symptoms of Meniere’s disease and is sometimes overlooked as a cause of treatment failure.
Meniere’s disease treatment
Treatment for Meniere’s disease begins with correctly diagnosing the condition. There are other disorders which can cause vertigo besides Meniere’s disease, like positional vertigo, and these must be ruled out. The diagnosis is made by history and through tests of hearing (audiogram), inner ear pressure (electrocochleography), caloric function, and others. MRI of the brain with contrast may be needed to rule out vestibular schwannoma (acoustic neuroma), a benign tumor of the balance nerve. Diagnosing Meniere’s can sometimes be difficult, and it is not always obvious whether a patient has it or not, although it usually can be more firmly established over time with repeated evaluations.
At the Shea Clinic, our approach is to aggressively treat patients, when possible, while they are in the early stages of Meniere’s disease with the intention of preventing or minimizing early damage to the delicate inner ear organs and thereby slow progression to a more advanced stage of disease. Although traditional conservative medical therapy for Meniere’s (low salt diet, diuretics, medication to control vertigo) is usually the first step in managing the condition for most patients, application of medication directly to the inner ear, known as intratympanic perfusion, is by far the most significant element in the approach to Meniere’s disease treatment in use at the Shea Clinic. In our opinion, at many other centers intratympanic perfusion is employed at a later-than-ideal time, after some permanent damage to the inner ear has already occurred. Our belief is that early intervention with intratympanic perfusion is the most effective way to prevent to progression of Meniere’s to its full-blown form for many patients.
The specialists at the Shea Clinic have many years of experience in diagnosing and treating Meniere’s disease. Dr. John Shea, Jr. (1924-2015) did a great deal of early work on developing intratympanic perfusion in the 1990’s, which is now considered state of the art treatment for Meniere’s disease and is the backbone of our treatment protocol at the Shea Clinic. Dr. Paul Shea was involved with a project while he was in medical school at Tulane University in which frogs had a medication called streptomycin (closely related to gentamicin) injected into their inner ears for the purpose of causing ablation (reduction) in hair cell and dark cell function. This research formed the basis for the modern intratympanic perfusion procedure that is currently used at the Shea Clinic in the treatment of Meniere’s disease and other inner ear disorders.
There is no cure for Meniere’s disease. It is a chronic condition, and the goal of treatment is to manage it as effectively as possible, reduce pressure in the inner ear, slow the progression to permanent inner ear damage and hearing loss, and mitigate its impact on the patient’s life.
Diet and medication regimens are individualized for each patient. Our goal is to minimize the amount of required daily prescription medication. Many patients respond to conservative treatment, but not all. We often recommend an early series of dexamethasone (steroid) perfusions, especially if sudden/fluctuating hearing loss or severe vertigo is present. This series of perfusions may be repeated months or years later as necessary. If the vertigo spells become more frequent and severe or if hearing continues to deteriorate, more aggressive treatment options may be appropriate.
Some patients may have ongoing unsteadiness and may benefit from vestibular rehabilitation (balance therapy), hearing aids, or cochlear implantation in cases where the hearing loss is so severe that hearing aids are no longer able to help. Other surgical procedures for Meniere’s disease include endolymphatic shunt/decompression and sectioning of the vestibular nerve, but these procedures are no longer performed at the Shea Clinic, as techniques and experience with intratympanic perfusion have proven to be safe, effective, and less invasive. At the Shea Clinic, the general approach to Meniere’s disease treatment is as follows:
- First Phase: Conservative Treatment
- Dietary modifications (reduced sodium and caffeine)
- Medications
- Diuretic (fluid pill) taken daily
- Oral steroids in a short taper or daily low dose “maintenance therapy”
- Medications for vertigo/nausea as needed (Valium, Zofran)
- Intratympanic perfusion with dexamethasone (steroid)
- Betahistine (possibly useful in mild cases)
- Daily exercise program, walking, increased activity
- Second Phase: When control is insufficient with conservative treatment
- Single intratympanic perfusion with low-dose gentamicin (10mg/ml)
- Repeated every 6 weeks until symptoms are controlled
- Gentamicin dose may be titrated up as necessary
- Hearing closely monitored and treatment stopped if decreasing
- Vestibular rehabilitation to improve balance function
- Third Phase: End-stage (“burned out”) Meniere’s disease
- Chemical Labyrinthectomy (intratympanic perfusion with “ablation-dose” gentamicin)
- Surgical Labyrinthectomy (surgical removal of balance organs)
- Cochlear implant to rehabilitate hearing
When you lose your hearing, those around you suffer the most.
Connect with your loved ones

